
[ad_1]
A sharp increase in the number of people presenting to Victoria’s already strained emergency departments for self-harm or in acute mental distress has prompted an almost $60 million boost to the state’s mental health services.
The number of people presenting to ED for self-harm across all age groups is up 9.5 per cent on the same time last year, Victorian Premier Daniel Andrews revealed today.
The rise has been even sharper in young people aged under 18 – up 33 per cent.
Overall, there has been a 23.3 per cent increase in mental health patients attending Emergency departments compared to last year.

“Emergency departments are busy at the best of times, particularly now in the height of a pandemic,” Victoria’s Minister for Mental Health Martin Foley said as he announced the funding boost.
“We want to make sure that we keep those people who need support for mental illness with the support that they need in the community – and that’s the main focus of today’s package is how to deal with the surge in demand.”
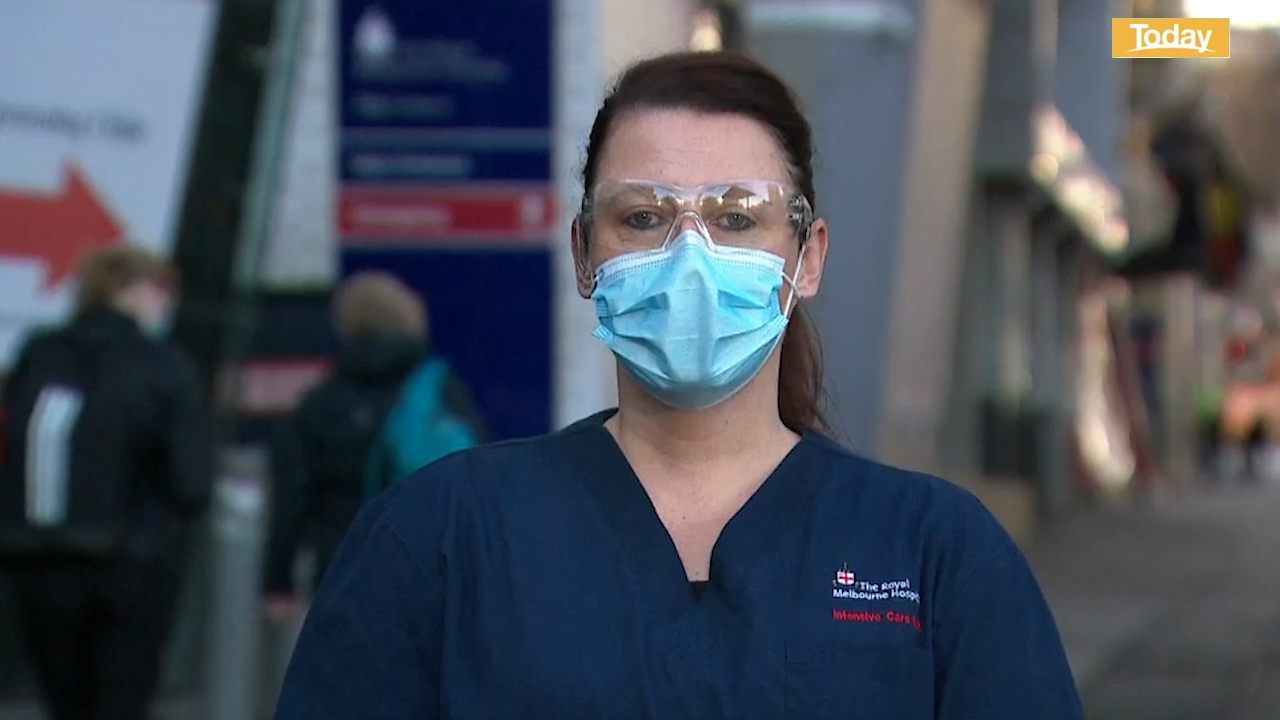
Mr Andrews announced the new measures today, noting that more counselling for frontline workers – including nurses, paramedics and police – would play a key part.
Of the new money, $250,000 will be allocated to increased counselling for nurses, midwives and paramedics.
“Many, many in our health team, particularly nurses, midwives, personal care workers, are doing it very tough,” Mr Andrews said.
“Particularly those nurses and personal care workers who have gone into aged care settings in fundamental crisis – you can’t unsee what you’ve seen.
“There is a degree of trauma, a degree of previously unknown levels of really, really challenging circumstances. It’s an incredibly difficult area in many of the settings.”
The Phoenix Trauma Centre will receive additional funds to support the mental health of police and paramedics on the front line of Victoria’s coronavirus fight.
There will also be additional training for Ambulance Victoria’s referral centre, which deals with medical concerns that go through the Triple Zero emergency line.
Minister Foley said this will be aimed at making sure “the mental health components of what goes through the triple zero line is dealt with in a way that again gets people the support, the information and the referrals that they need closer to them and in their community”.
Among the new measures is a fast-tracking of two key recommendations made by the Royal Commission into Victoria’s Mental Health System: more in-patient beds for acutely unwell mental health patients; and the state-wide implementation of the Hospital Outreach Post-Suicidal after Engagement (HOPE) program.
This will see an additional 144 new in-patient beds for acutely unwell mental health patients in the Barwon region and Melbourne’s northern and western catchments.
In addition, the HOPE program’s rollout to the last seven of the 23 health regions yet to receive those services will be brought forward.
The program provides support to those who have either attempted suicide or who have expressed an intention of doing so.
“That program is an amazing program and one that Victoria leads the nation with,” Mr Andrews said.
“Anyone with suicidal thoughts, anyone who has tried to act on those thoughts, gets that wrap-around service, personalised and local in a familiar environment in a nonclinical environment wherever possible.”
Some of the $59.7 million in new funds will be allocated to help local mental health support services open seven days a week with extended hours, allowing those in need to access those services rather than present at hospitals.
Additional funds will also be allocated to increased psychiatric support for patients, allied professional help support, data collecting and record keeping.
There will also be more support for not-for-profit Headspace, to more assertively engage with the acutely unwell in the community, especially people.
[ad_2]
Source link