
[ad_1]
Pneumonia is likely one of the main causes of hospitalization amongst adults. With the perpetual push towards value-based care and different fee fashions that incentivize suppliers to enhance care and decrease prices, pneumonia’s prevalence makes it a very good candidate for episode‐based care models. As an acute an infection, pneumonia could also be a extra pure match for episode-based fee than hospital admissions for exacerbations of continual situations, akin to coronary heart failure. But in follow it’s not that straightforward, and there are obstacles to fee reform for pneumonia care.
While pneumonia is frequent, it usually presents with different situations that may make designing a profitable payment bundle troublesome. In a brand new study titled “Pneumonia is Not Just Pneumonia,” LDI Executive Director Rachel M. Werner, Senior Fellow Amol S. Navathe, and colleague Jessica T. Lee discover that comorbid situations related to pneumonia complicate the fee panorama for sufferers and suppliers.
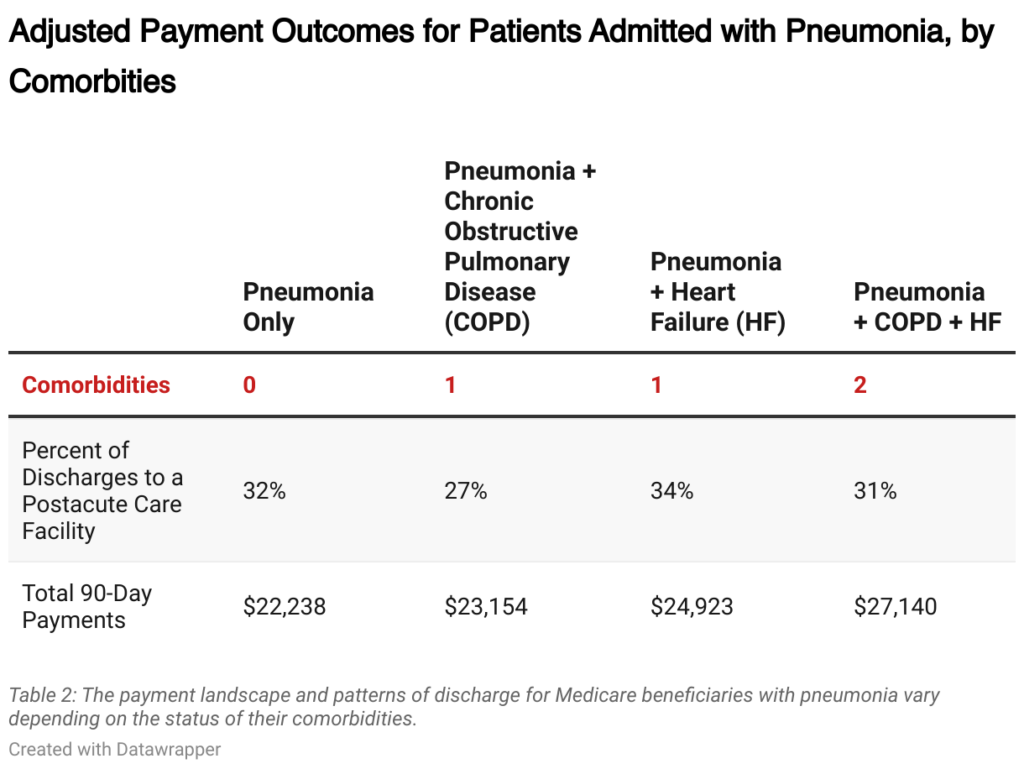
Common comorbidities of pneumonia, like chronic obstructive pulmonary disease (COPD) and heart failure, play a major function in impacting therapy patterns and due to this fact the prices of take care of sufferers with pneumonia. The investigators needed to know how comorbidities influenced using postacute care, such because the care offered by nursing services, because it accounts for a big a part of the prices and/or financial savings in varied bundled payments.
To discover the incidence of comorbidities for pneumonia and their affiliation with prices and postacute care use, investigators examined hospital discharges of Medicare beneficiaries hospitalized for pneumonia, with and with out these comorbidities, utilizing Medicare claims knowledge from 2010-2016.
Investigators discovered that, as hypothesized, sufferers with COPD and/or coronary heart failure comorbidities had larger whole funds within the 90 days after hospitalization. Unsurprisingly, the funds had been highest amongst sufferers with extra comorbidities in comparison with these with fewer.
Although, surprisingly, extra comorbidities didn’t all the time translate into extra time in institutional postacute care: Compared to sufferers with solely pneumonia, sufferers with pneumonia and COPD—or with pneumonia, COPD, and coronary heart failure—had been much less prone to be discharged to a facility, and those that had been discharged to a facility spent fewer days there.
According to co-investigator Jessica T. Lee, “It actually makes clinical sense that patients who still qualify for hospital admission without the most common comorbidities might actually be sicker in ways that are hard to see in claims data, such as being unable to eat enough at home while they have pneumonia, factors that would influence their need for help after discharge. But that may mean that diagnoses that appear to be acute conditions, like infections, may require care that more reflects the patient status than the admission diagnosis, even when you adjust for comorbidities.”
These outcomes spotlight how a affected person with pneumonia’s comorbid situations can considerably affect their prices and course of care, providing worthwhile perception for planning value-based care interventions. Investigators advocate that with a view to design the simplest different fee fashions for frequent situations akin to pneumonia and different situations with excessive hospitalization charges, well being care leaders and policymakers ought to contemplate comorbidities along with different affected person traits.
The research, “Pneumonia is Not Just Pneumonia: Differences in Utilization and Costs with Common Comorbidities,” was revealed on October 10, 2023 within the Journal of Hospital Medicine. Authors embody Jessica T. Lee, Amol S. Navathe, and Rachel M. Werner.
Author

More on Health Care Access & Coverage

Texas Abortion Case Shows the Limits to Exceptions in Abortion Bans
People Whose Babies Will Surely Die Should Be Able to Choose Their Care

For-Profit Hospitals Admit at Higher Rates from Emergency Departments Than Nonprofits
LDI Fellow’s Study Supports Federal Probes of Hospitals for Over-Admitting Patients

Val Arkoosh, Pa.’s Human Services Head, Describes Her Strategy for Change
The DHS Secretary Cites Key Moves in Medicaid at an LDI Event

Nonprofit Hospitals Are Hounding Poor People for Money and Failing to Serve Patients’ Interests, News Reports Show
Here’s How to Get Them to Refocus on Their Communities Instead of Profits

Will Over-the-Counter Access Increase Availability of an Overdose-Reverser and an Oral Contraceptive?
Probably Not: If the Past Is Any Guide, Cost and Access Will Likely Stand within the Way

Americans May Support Medicaid Work Requirements But Not Efforts to Exclude People for Noncompliance
Survey Shows Surprising Agreement Among Groups Regarding Health Care Coverage Policies
[adinserter block=”4″]
[ad_2]
Source link