
[ad_1]
Clinical file
In August 2022, a 19‐12 months‐previous male scholar with a historical past of bronchial asthma and nut anaphylaxis was taken by ambulance to hospital when he was discovered unresponsive with vomitus and faecal soiling after someday of lethargy and sore throat. On arrival, his blood strain was unrecordable, coronary heart fee was 110 beats per minute, respiratory fee 55 breaths per minute, oxygen saturation 63%, temperature 36°C, and the Glasgow Coma Scale rating was 6. He had no neurological indicators, no meningism and no rash, and was updated with immunisations, together with meningococcal C and ACWY vaccinations.
Investigations revealed hyperlactataemia 7.8 mmol/L (reference interval [RI], < 2 mmol/L), neutrophilia 27 × 109/L (RI, 1.7–7 × 109/L), anaemia 104 g/L (RI, 130–180 g/L), thrombocytopenia 124 × 109/L (RI, 150–450 × 109/L), C‐reactive protein (CRP) 233 mg/L (RI, < 3.0 mg/L), bilirubin 25 μmol/L (RI, < 20 μmol/L), and worldwide normalised ratio 2 (RI, 0.8–1.3), precluding lumbar puncture. Serum creatinine and transaminases have been regular. A nasopharyngeal swab for extreme acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), influenza virus and respiratory syncytial virus by polymerase chain response (PCR), and pneumococcal and Legionella urinary antigens have been adverse. He was handled for septic shock with intravenous antibiotics (flucloxacillin, gentamicin), hydrocortisone, noradrenaline, and fluids, and was intubated and admitted to the intensive care unit. Computed tomography revealed bilateral pulmonary floor glass opacities. On infectious illnesses session, toxin‐mediated shock and meningococcal aetiology was suspected, which prompted droplet precautions, public well being unit notification, and a change in antibiotics to intravenous ceftriaxone and clindamycin. Gram‐adverse diplococci have been remoted from blood tradition at 17 hours and have been optimistic for Neisseria meningitidis serogroup B on blood PCR (ctrA and porA genes). Clinical enchancment led to extubation 30 hours after admission. The affected person skilled retrograde amnesia with in any other case full neurological restoration and determination of fevers by day 4. Treatment was accomplished with 5 days of ceftriaxone.
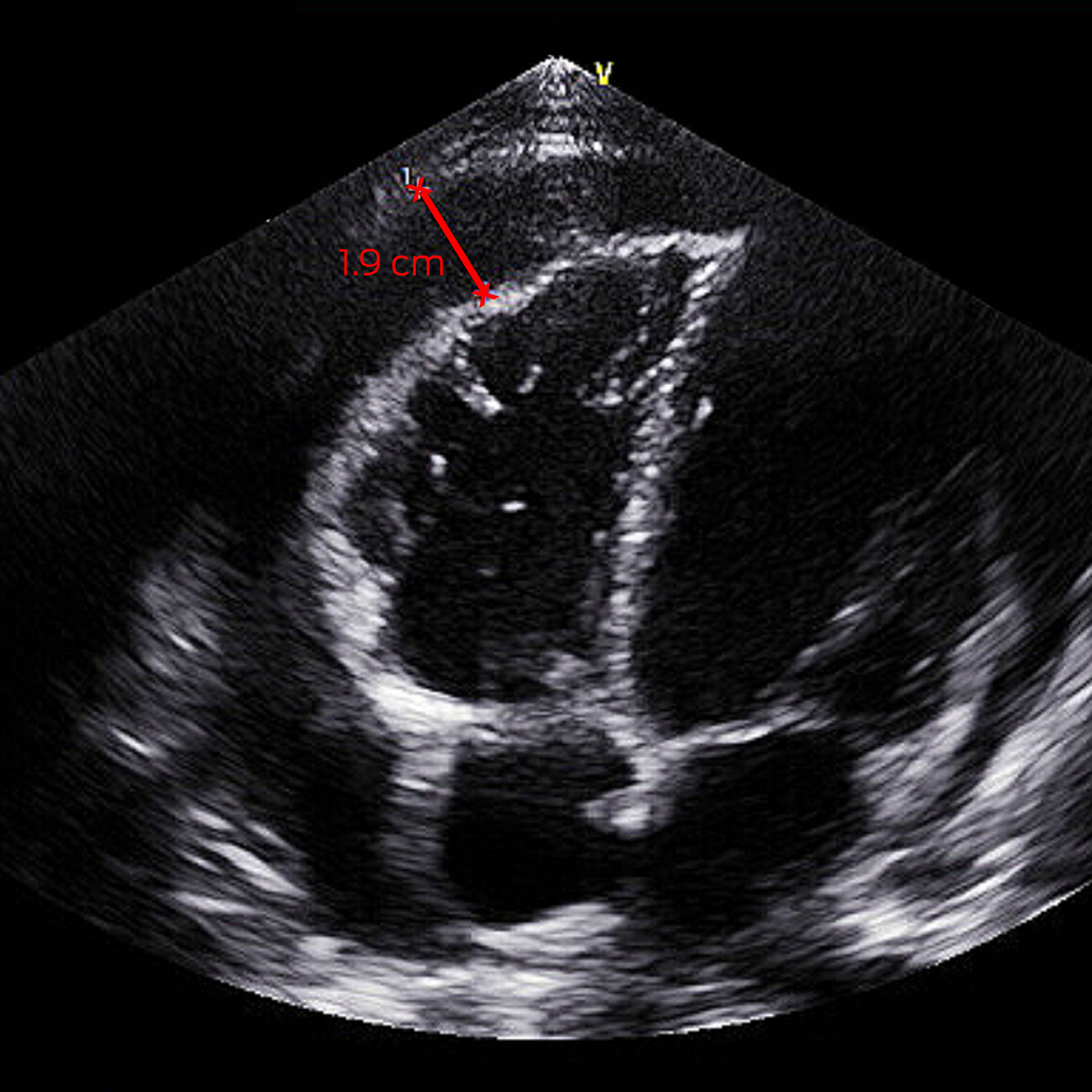
On day 5, his fevers recrudesced to 39°C with a brand new pericardial rub and anterior T‐wave flattening on electrocardiogram. Investigations demonstrated elevated troponin T 193 ng/L (RI, < 14 ng/L), CRP 65 mg/L, and whole haemolytic complement > 1000 U/mL (RI, < 1000 U/mL). Septic display screen was adverse. Transthoracic echocardiography (TTE) confirmed a 0.5 cm pericardial effusion growing to 1.9 cm (Box 1). He was handled for reactive meningococcal pericarditis with common ibuprofen and colchicine, with decision of fevers and enchancment in inflammatory markers, and he was discharged 5 days later. He had adverse human immunodeficiency virus (HIV) serology and regular complement research after restoration. Minimal effusion on TTE by week 6 prompted transition to colchicine monotherapy, which was ceased at week 10.
The public well being unit initiated contact tracing on scientific suspicion of invasive meningococcal illness (IMD) earlier than microbiological affirmation. Seven increased danger contacts have been recognized and acquired ciprofloxacin clearance antibiotics and knowledge on IMD. Information was supplied to decrease danger contacts. No additional instances of IMD have been recognized.
Discussion
IMD is brought on by Neisseria meningitidis, an cardio gram‐adverse diplococcus that colonises the human nasopharynx. Transmission happens by respiratory droplets and extended publicity with asymptomatic carriers. Pathogenic strains produce a polysaccharide capsule that inhibits complement‐mediated lysis, enhancing intracellular survival and bloodstream invasion.1 Incubation is one to seven days and infrequently as much as ten days, adopted by an infection starting from gentle respiratory sickness to IMD with septic shock, suppurative meningitis, or each. Secondary disseminated intravascular coagulopathy produces a petechial rash, which might proceed to tissue infarction.2 Diagnosis is confirmed by PCR take a look at or microscopy and tradition of N. meningitidis from a sterile website.2 Presentations could also be atypical and lack overt meningism or rash, as on this case.
IMD happens seasonally throughout winter and spring in a bimodal age distribution, with highest incidence in kids aged beneath 5 years and adolescents aged 15–19 years.2 Risk components embrace immunosuppression, terminal complement pathway deficiencies, smoking, and up to date higher respiratory tract infections with increased charges in Aboriginal and Torres Strait Islander folks.1,2,3 IMD is related to 10% mortality, with 10–20% of survivors having long run issues.2 Autoinflammatory issues from kind III hypersensitivity reactions, notably pericarditis, arthritis, pleuritis and vasculitis with secondary fever, can happen between day 4 and 14 through the restoration part.1,2 Unrecognised, outcomes for reactive meningococcal pericarditis could be poor. Treatment consists of non‐steroidal anti‐inflammatories, colchicine, and, often, corticosteroids and pericardiocentesis.1
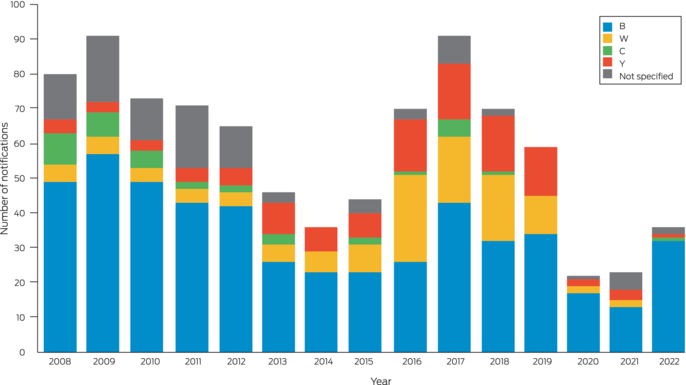
In Australia, IMD is clinician‐ and laboratory‐notifiable on a excessive index of suspicion. It is uncommon, with annual incidence reducing from 3.5 instances per 100 000 in 2002 to 0.8 per 100 000 inhabitants in 2019, with serogroups B, C, W and Y inflicting the vast majority of instances.3,4 In 2018 and 2019, serogroup ACWY vaccination was added to the National Immunisation Program for infants and adolescents. This adopted preliminary jurisdictional‐degree applications in response to serogroup W outbreaks and will increase in serogroup Y illness. Serogroup B has since change into predominant nationally and in New South Wales (Box 2).5 In 2020, meningococcal B vaccination was added to the National Immunisation Program for Indigenous kids and folks with medical situations related to elevated danger of IMD.3
Incidence additional declined to 0.3 per 100 000 inhabitants in 2021,6 doubtless from measures to scale back SARS‐CoV‐2 transmission.4 Minimal influenza virus transmission doubtless additionally contributed, as antecedent influenza an infection is a danger issue for IMD.4 With the comfort of measures associated to the coronavirus illness 2019 (COVID‐19) pandemic, the specter of IMD is re‐rising. This case highlights the significance of early analysis, immediate public well being notification, and recognition of atypical shows and critical sequelae reminiscent of pericarditis.
Lessons from follow
- Invasive meningococcal illness (IMD) is re‐rising after the comfort of coronavirus illness 2019 (COVID‐19) public well being measures.
- IMD might current atypically with out rash or neurological indicators.
- Recovery from IMD could also be difficult by autoreactive sequelae, together with pericarditis.
- Early scientific recognition and public well being notification is crucial for the administration of IMD.
- Meningococcal B vaccine is free beneath the National Immunisation Program for Aboriginal and Torres Strait Islander kids beneath two years of age, and folks of all ages with asplenia and hyposplenia, complement deficiency, and people receiving remedy with eculizumab.
Box 1 – Transthoracic echocardiogram off‐axis 4 chamber view with pericardial effusion measuring 1.9 cm
Box 2 – Invasive meningococcal illness notifications in New South Wales residents, by 12 months of onset and serotype (2008–2022)5
[adinserter block=”4″]
[ad_2]
Source link