
[ad_1]
To keep our community informed of the most urgent coronavirus news, our critical updates are free to read. Ongoing coverage is available to subscribers. Subscribe now for full access and to support our work.
The alarms finally went off at San Antonio’s Metropolitan Health District on June 10.
Until then, officials were satisfied with the number of case investigators who were calling COVID-19 patients to identify their close contacts and control the spread of the disease.
Read Emerick’s June 23 email on need for more volunteers
Only 25 investigators were working at that point, a fraction of the 175 that a panel of health experts had recommended in April. Nonetheless, a Metro Health working group reported June 8 that the agency’s contact tracing capacity was “in good shape.”
Two days later, the tone had changed dramatically.
“We have seen an increase of over 500 positive COVID-19 cases in just 4 days,” Jennifer Herriott, deputy director of Metro Health, wrote in an email asking for 30 staff members to help with case investigations. “I know this may sound crazy and unexpected, but this is REALLY important and REALLY urgent. … And no, this is unfortunately not a joke.”
To others, the emergency was not unexpected. Despite repeated warnings that Metro Health did not have enough people to track the spread of COVID-19, leaders were slow to build up their fleet of investigators as the virus began to ravage Bexar County.
Now, at least 2,692 cases are backlogged for investigation, and Metro Health officials have written off an untold number from before June as pointless to pursue.

This account is based on interviews with city officials and public health experts and a review of email traffic between Metro Health leaders, elected officials and others through the month of June. In all, the Express-News examined 6,000 pages of emails obtained through a Texas Public Information Act request.
Cherise Rohr-Allegrini, an epidemiologist who served on the panel that recommended 175 investigators in April, watched with dismay for weeks as the agency waited to bolster its workforce for investigations, a primary function of health departments charged with controlling the spread of any contagion.
For each new COVID-19 case, an investigator is assigned to call the patient and collect information on any close contacts, defined by the Centers for Disease Control and Prevention as “someone who was within 6 feet of an infected person for at least 15 minutes starting from 48 hours before illness onset until the time the patient is isolated.”
The investigators share that information with contact tracers, who warn the close contacts that they’ve been exposed to the virus and encourage them to get tested and to self-quarantine.
Until the surge in June, Metro Health was adhering to what it called the “70-15-90” rule: a gradual accumulation of 175 case investigators over four months as cases increased. The formula called for training 15 new investigators should COVID-19 cases reach 70 a day for a sustained period — and deploying them once the growth in cases reached 90 per day.
“It was a ridiculous plan,” Rohr-Allegrini said. “It made no sense in terms of outbreak investigation. Once you start getting into more than 20 or 30 a day, those numbers start doubling. And anybody who knows epidemiology would know that. You don’t wait until after the outbreak starts to get people trained.”
Infections here began to show up in March and remained mostly in the double digits until a steady rise in cases started in late May.
Dawn Emerick, the former director of Metro Health who resigned last month, had asked Rohr-Allegrini to recruit and train more than 100 case investigators in April. The epidemiologist began to coordinate UT School of Nursing students and others to volunteer for the critical work.
About two weeks later, Emerick halted those plans after getting push-back from Assistant City Manager Colleen Bridger, with whom she would clash bitterly throughout her six-month tenure at Metro Health. Bridger took over as director of the agency after Emerick’s June 25 resignation.
“Dr. Bridger wants to do the recruiting and training of contact tracers completely different than the original vision I had,” Emerick wrote Rohr-Allegrini on May 11. “This changes the way we hire, training approach … everything. Right now — currently — we do not need to rush to train anyone. Case tracing capacity is OK at Metro Health.”
Emerick declined to comment for this article.
Rohr-Allegrini knew then that capacity was not OK.
“It never ramped up,” she said. “If we had set it up within that week and been ready by May 15 like we intended, we would have a much better handle on the situation.”
Pressure builds
With COVID-19 now out of control — hundreds of daily cases have become the norm in San Antonio, and more than 300 people have died from the disease — Metro Health has made some progress on case investigations and contact tracing.
In May, the agency outsourced its contact tracing to eMocha, a mobile technology company. But that service had reached only 1,177 residents June 15, records show. Metro Health recently expanded its contract with the firm, increasing the number of eMocha contact tracers from just three to 12, Bridger said.
Next week, the health agency will begin to integrate its contact tracing into a statewide system called Texas Health Trace.
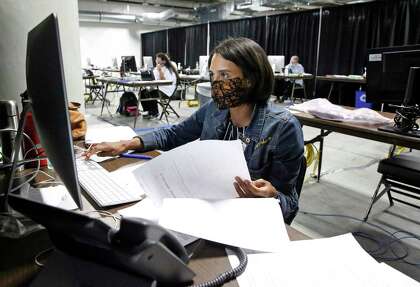
Metro Health has moved 116 case investigators, or about 70 a day, into a large space at the Alamodome. Most of them are Metro Health employees. By the end of August, a $2 million contract with the UTHealth School of Public Health will yield a total of 400 case investigators — 200 from the university and 200 from the Metro Health — as well as 175 contact tracers.
“That should be more than enough,” Bridger said. “Unless we start having more and more days where we have 2,000 cases, that should be more than enough.”
Read Colleen Bridger’s June 10 email on case backlog
The 400 investigators gradually will ramp up in groups of 50 over the next month, Bridger said.
“When we are fully, fully up and running between UT and the city, it will be 400,” she said. “Now, if our case numbers are down — and that’s another reason we’re doing it in clumps of 50 — if our case numbers start to go down like we hope they will, then we won’t bring on more people than we need. That’s the other thing to remember. If we’re having 400 cases a day, we don’t need 400 case investigators.”

Rohr-Allegrini, who’s now co-chair of a Metro Health contact tracing work group, bristled at that strategy.
“You don’t just have the 400 (cases) from today. You have the (thousands) from the past month that you don’t have investigated,” she said. “We have to be careful not to repeat the same mistake as we did earlier by not hiring people when we have the chance.”
Despite the backlog, City Manager Erik Walsh said a measured approach to bringing on investigators was appropriate.
“But it has to be an engine that can be throttled quickly,” Walsh said. “And I think we’ve probably seen in the midst of everything that happened in June, as cases started to go up and that pressure started building within the public health world here locally, I think we all asked ourselves, ‘If schools open up, are we going to see another spike 30 days later in October or November? And how do we start to plan for those peaks?’
“I don’t think everybody anticipated the peak.”
‘Sense of anxiety’
Health officials across the country — not just in San Antonio — have been overwhelmed by surges in COVID-19 cases.
Before the novel coronavirus emerged this year, health departments in America largely were equipped to contain outbreaks of other diseases, said Dr. Oscar Alleyne, chief program officer for the National Association of County and City Health Officials.
“We have not previously had to ramp up our workforce to the capacity where we’re seeing now,” Alleyne said. “The public health governance enterprise has never had to stand up to the volume and capacity that is going to be necessary for containing this disease.”
In collaboration with the Fitzhugh Mullan Institute for Health Workforce Equity at George Washington University, NACCHO created an online tool that estimates how many case investigators and contact tracers are needed to control COVID-19 in counties across the nation.

In Bexar County, given the current outbreak, 540 case investigators are needed, according to its Contact Tracing Workforce Estimator.
Last month, city leaders were flummoxed by a growing backlog of cases that had yet to undergo investigation or contact tracing.
“The number of people pending contact tracing appears to be 350. Is that true?” Bridger emailed Emerick on June 10. “Why is it so high? I thought we had a bunch of contact tracers trained and ready to go. … We need to get that number down.”
Emerick reacted the next day.
“Starting immediately we are redeploying Metro Health staff, SA Fire and volunteers to assist with case investigations and contact tracing,” she wrote to employees June 11. “Unfortunately, we are considering this the beginning of a second wave.”
In another email, Emerick wrote, “We are seeing signs of a second wave and it has me and my team spinning.”
Leaders at the highest levels of the city’s COVID-19 response also were alarmed. On June 13, Walsh called a meeting with Emerick, Bridger, hospital leaders, Fire Chief Charles Hood, Mayor Ron Nirenberg and Bexar County Judge Nelson Wolff.
“There is a sense of anxiety among this group,” Emerick told her team that day.
Read Jennifer Herriott’s urgent call for staff
That same day, Emerick sent an email arguing that Metro Health should stick with eMocha, at least temporarily.
“I think there’s significant value in continuing to use them for at least another 30 days,” Emerick wrote. “The problem they are solving for us — right now — is taking on the contact tracing load so we can focus on case investigations. The state’s system isn’t up and running yet and it would be mistake to turn a contact tracing resource away right now.”
Rita Espinoza, Metro Health’s chief of epidemiology, agreed — with a caveat.
“The one thing that I feel was overlooked was a transition plan on what to do once the (eMocha) pilot ended,” Espinoza wrote.
‘Not enough’
Four days after Herriott first sounded the alarm, she sent an email June 14 urging Metro Health employees to work overtime hours on case investigations and contact tracing.
To assist, Emerick also began to pull employees from other Metro Health divisions, including epidemiologists who normally would be tracking the spread of sexually transmitted diseases and tuberculosis. She asked UT Health and the University of the Incarnate Word to send volunteers to help out.
The need also was apparent to outsiders.
On June 19, a sales manager for National Commercial Collections Group, a debt collection agency, pitched the company to Emerick as ideal to take on contact tracing — a proposal Emerick forwarded to her staff.
Despite the pressing need to bolster the number of people tracking the spread of the virus, Bridger twice denied Emerick’s requests to pull employees from other city departments to help with the investigations, Emerick wrote in a June 23 email.
“While I know that we are doing the best we can, while I know all of us are putting new systems in place and directing staff to help, it’s not enough and it’s taking too long,” Emerick wrote to two Metro Health officials. “I am extremely uneasy with the growing number of back-logged cases. It’s ultimately my responsibility to fix this and it’s concerning to me that we are not pulling in all resources and options.”
Case investigators have had a hard time getting people who have tested positive for the virus to return phone calls. Upon hearing that people under age 25 were particularly bad about returning calls, Emerick on June 25 — “joking, not joking” — floated the idea of tricking younger people into answering the phone by using misleading caller ID names.

Among the names Emerick suggested on the same day that she resigned: “Mom,” “Dad,” “Free Beer,” “Work,” “Tinder,” “Netflix,” “University of Texas” and “Matthew McConaughey.”
‘A lot of mistakes’
Since Emerick’s departure, Metro Health has applied a more straightforward solution: Calls by case investigators now are identified as coming from the “SA Health Department.”
Asked whether more patients are answering calls, Bridger said: “It has gotten a little bit better.”
She added, “Clearly, there were a lot of mistakes that everybody made. But none of it was intentional, and all of it was to make the next iteration and the next iteration better.”
This month, Bridger sent a memo to the city manager, mayor and other members of city council outlining Metro Health’s progress in the COVID-19 response. She acknowledged numerous “challenges” during Emerick’s tenure, including “insufficient staff to do case investigations/contact tracing,” resulting in delays “beyond the infectious period of 14 days.”
Among the solutions, Bridger wrote that Metro Health has flipped its own case investigation process so the newest cases are contacted first.
Bridger noted in the memo that nationally, less than 50 percent of case investigations are completed.
“I understand 100 percent may be an unrealistic goal,” said District 7 Councilwoman Ana Sandoval, chair of the council’s Community Health and Equity committee. “But if there’s anything we can do to make sure that we’re in contact with everyone who tested positive and contain that disease, of course we should try to do it.”
Sandoval, who has a master’s in public health from the Harvard School of Public Health, said she had difficulty grasping the now-abandoned “70-15-90” formula. She said Emerick told her that the formula was designed to avoid overwhelming Metro Health.
Initial plans to ramp up the number of case investigators were based on projected peaks of 75 new cases a day, Sandoval said, citing past remarks from Bridger.
On Thursday, the county reported 1,078 new cases.
Nirenberg said the necessary workforce has clearly expanded far beyond the city’s previous goals.
“My concern is that if we’re not getting the job done with the amount of contact tracers we currently have, then we need more,” Nirenberg said. “That is a pretty simple formula. How we bring them on is an operational issue. But let’s get the job done.”
Rohr-Allegrini, the epidemiologist, said it might be too late.
“My goal as a public health professional is not to focus on all the screwups that already happened, but to focus on moving forward,” she said. “But that also means understanding the mistakes so we don’t repeat that. Looking back, our mistake was not hiring the first batch of 175 in May. And now we’ve lost two and half months.
“Now we have to ramp up at rapid speed. We are so far behind, we’re never going to catch up. But it’s not OK to just let the fire burn.”
Joshua Fechter is a staff writer covering San Antonio government and politics. To read more from Joshua, become a subscriber. jfechter@express-news.net | Twitter: @JFReports
[ad_2]
Source link