
[ad_1]
Every year, around 120,000 people die prematurely from noncommunicable diseases (NCDs) in Sri Lanka. Despite its robust health system, gaps exist in the training and mentoring of health professionals to address NCDs in their services, resulting in avoidable
diseases, poorer care and worse health outcomes for patients.
Recognising that tackling these gaps could improve patient care, and responding to the challenges of the COVID-19 pandemic, Sri Lanka has established a new virtual ‘hub and spoke’ training module to reach health care professionals working
on NCDs.

Credit: WHO
Facing up to NCDs
Thanks to its well-established health system, Sri Lanka has achieved indicators of health status and service coverage well above its neighbouring countries. The country has a well-planned network of Medical Officer of Health units, providing comprehensive
and evidence-based services, integrated with local public health inspectors and midwives at the grassroots level. The high standards of this integrated health delivery system has enabled Sri Lanka to achieve strong health gains at low cost.
However, NCDs are posing an ever-increasing threat to these health systems. Currently, more than 80% of all deaths are attributed to NCDs – resulting in approximately 120,000 premature deaths every year. Cardiovascular diseases (CVDs) account for around one-in-three of these deaths, followed by cancers, diabetes and chronic respiratory diseases.

Credit: WHO
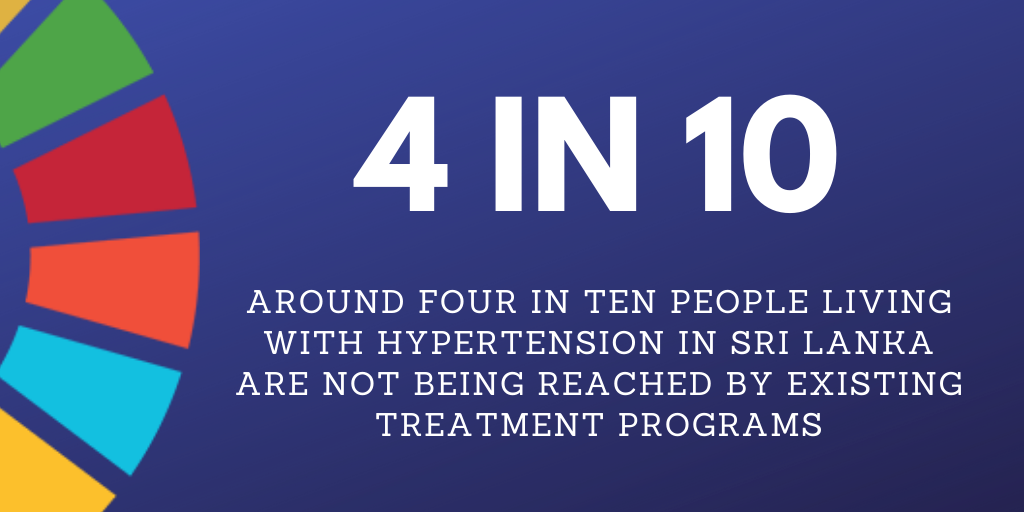
As well as challenges posed by an ageing population, risk factors for NCDs are also highly-prevalent. One quarter of all Sri-Lankan’s currently live with hypertension, and one in twelve with diabetes. Almost three-in-ten men currently smoke, while
average salt consumption for both men and women is double the WHO ’s recommendation of 5g per day.
Dr. Nalika Gunawardena, National Professional Office, WHO Country Office, Sri Lanka, explains to us why acting on NCDs is so important:
“Noncommunicable diseases are an extremely pressing concern for our health. But they are also a significant challenge for Sri Lanka’s development, with NCDs driven by underlying social, economic, political, environmental and cultural factors broadly known as ‘social determinants’.
Health-promoting partnerships are a vital way for Sri Lanka to address the social determinants of NCDs. This project to train and mentor staff working in primary care to screen, diagnose, treat and refer for NCDs is one such extremely important partnership. WHO is committed to continued local support, to ensure the human and financial burden of NCDs do not undermine development gains”.
Despite the availability of free health care to all, around 40% of people living with common NCDs in Sri Lanka are currently not diagnosed or treated. And among those treated, data show far too many do not achieve the desired health outcome.
Training in NCDs: a vital piece of the puzzle
Recognising the critical importance of NCDs to universal health care, the Sri Lankan Ministry of Health has introduced several initiatives to aim for the WHO’s target of a 25% reduction in premature NCD mortality by 2025, and the UN Sustainable
Development Goals. These include:
- delivering essential NCD screening in its Healthy Lifestyle Centres and Well Women Clinics;
- focusing on providing appropriate treatments at different levels of care;
- improving cancer detection and mental health services.
While progress is being made, the coverage of these programmes remains low with a slow pace of adoption. And ultimately, their success relies on giving health workers and facility managers the skills and mentoring they need to create positive changes
to health service delivery.
Credit: WHO
Traditionally, the Ministry of Health has adopted a face-to face model to train its workforce and build capacity by cascading information. While this training is effective and extremely helpful, it can be tricky to reach the right staff at the right
time, leading to inconsistent levels of knowledge in how best to respond to NCDs.
Despite the emerging evidence of their effectiveness, using virtual technology tools to train and mentor health staff were underused in Sri Lanka. And with new challenges posed by the COVID-19 pandemic, the need to embrace innovative training
and mentoring models was urgently felt by all.
Dr Vindya Kumarapeli, Director for NCD at the Sri Lankan Ministry of Health, explains this urgency:
“Before COVID-19, we had not really explored the take up of online and distant learning methods for in-service training and mentoring in Sri Lanka. This project provided us with a good opportunity to equip ourselves with the technological support needed to do so. This will allow us to give our health workers the best-quality training, and boost the reach of our training”.
Fixing these challenges
Boosting capacity to deliver digital training and mentoring for those working on NCDs was a key issue of need. Working with the Ministry of Health, this project funded by the Denmark Government set the goal to establish a learning management system
from which this virtual capacity building could begin.
This system focused on establishing a ‘hub and spoke’ model, where the Ministry of Health’s NCD Directorate provides the central training function, and the staff of nine institutions spread across Sri Lanka’s nine provinces receive training and mentorship from the Ministry.
By building the capacity of technical staff within the Ministry of Health to use virtual training alongside face-to-face courses, developing a structure of courses, and trialling the training across nine sites in each province of Sri Lanka, there is huge potential for the project to be scaled up in future if successful.
The result: a much-needed training model with room to grow
Given the pressing need to establish virtual training, with COVID-19 limiting opportunities for face-to-face meetings, considerable progress has been achieved in just three months.
Perhaps the biggest logistical challenge, the much-needed institutional arrangement to create a ‘hub and spoke’ model has been set up, including supplying video conferencing facilities and IT infrastructure needed to deliver NCD service training.
To serve this model, WHO has worked closely with the NCD Directorate to provide the best-quality resource possible for health staff. This has included identifying the training areas of most need, being considerate of the needs of trainees and trainers and understanding their motivations, and adapting and creating new modules for virtual delivery.
Dr Chithramali Rodrigo, a postgraduate trainee in Community Medicine, explains how the new training may help her:
“Undergoing online in-service training and participating in online review meetings are new experiences for me. Previously all the training I had undertaken were face to face.
Due to the threat of COVID-19, we could not continue this. While adapting to the ‘new normalcy’ I consider the online mode of training to be very effective and efficient. It will help me to keep updated with the latest evidence and guidelines, and to enhance my work on caring for the community”.

Previously, NCD training was conducted face-to-face: dancing optional to keep up physical activity! Credit: Mr Ruwan Bandara, WHO Country Office Sri Lanka
Digital training creates new opportunities to reach health workers on the frontline, where this training would have previously been face-to-face, and paused indefinitely because of COVID-19.
As one example, Sri Lanka’s existing technical package to improve cardiovascular health (HEARTS) can now be delivered through an online, self-learning training program, creating potential to widen access and improve care outcomes.
The next step: what will happen now?
Supporting those working on the frontline to prevent, treat and manage NCDs is crucial for the quality of life of the millions of Sri Lankan people currently living with these diseases. Learnings from the COVID-19 pandemic indicate that digital
health will play an increasing role in how this support is delivered.
We will be closely following the development of the new virtual training model, and it will be vital to learn from experiences of health staff and trainers, to understand how to best improve knowledge and practice changes. Understanding the motivations
for those who participate is an important aspect, and we are exploring the opportunity to gain accreditation for NCD courses, giving people the chance to receive a diploma-level certificate for their participation.
As well as the clear benefits of improving the integration of NCDs in health systems delivery, the project creates several future opportunities for the health of the Sri Lankan population. In addition to a new digital module on cardiovascular health, plans are afoot to design new NCD-related virtual training and mentoring modules.
What’s more, there are added possibilities across the region, with the Sri Lankan Government recently participating in webinars with colleagues in Bhutan and Nepal to share learnings on designing a virtual training program.
Better training in how to prevent, diagnose, treat and manage NCDs in health systems leads to better patient outcomes. And by mentoring the emerging NCD leaders of tomorrow all across the country, we hope this project can enable innovative ideas to grow.
Across the Global Week for Action on NCDs (7-13 September), we are sharing stories from the field about why acting on NCDs is so important. These stories have emerged from a recent project funded by the Government of Denmark. Today’s story was written by Dr Nalika Gunawardena, Dr Vindya Kumarapeli and Mr Daniel Hunt.
[ad_2]
Source link