
[ad_1]

Demonstrators outside PhRMA headquarters in Washington, D.C., protest lobbying by pharmaceutical companies to keep Medicare from negotiating lower prescription drug prices.
Saul Loeb/AFP via Getty Images
hide caption
toggle caption
Saul Loeb/AFP via Getty Images
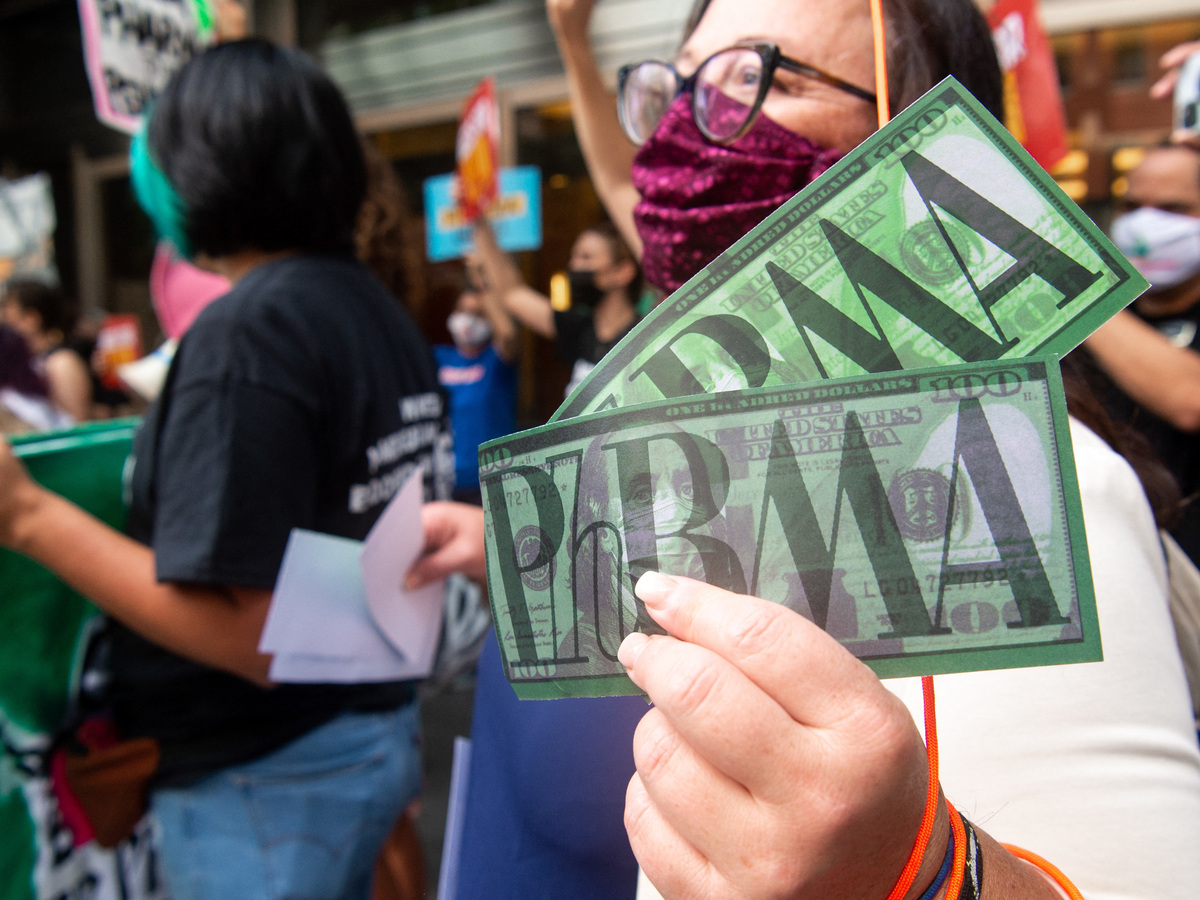
Demonstrators outside PhRMA headquarters in Washington, D.C., protest lobbying by pharmaceutical companies to keep Medicare from negotiating lower prescription drug prices.
Saul Loeb/AFP via Getty Images
Americans pay way more than people in other countries do for prescription drugs. This drives voters crazy, and although lawmakers have been vowing to do something about it for decades, they haven’t made much progress.
That could change as soon as this week. The Inflation Reduction Act – hashed out by Senate Majority Leader Chuck Schumer, D-N.Y., and Senator Joe Manchin, D-W.V. – includes several provisions around drug prices and health insurance. The Senate is planning to bring the bill to a vote Saturday, and it appears on track to get through Congress and be signed into law by President Biden.
This is all music to the ears of patients who’ve been burdened by high-priced drugs for years.
“The proposal to limit out-of-pocket expenses that’s on the table right now would absolutely make a huge difference in my life,” says Medicare recipient Bob Parant, 69, of Westbury, New York. He has Type 1 diabetes and pays about $5,000 out of pocket for insulin each year, on top of thousands more for a heart medicine.
Here are details about that proposal and others in the bill, and answers to some frequently asked questions.
What exactly is Congress changing about drug prices?
For the first time, the federal health secretary would be able to directly negotiate the prices of certain expensive drugs each year for Medicare. This starts in 2026 with 10 drugs and increases to 20 drugs by 2029. To qualify for negotiation, the drugs would have to be on the market for several years.
Then there’s the proposal Parant is most excited about: People on Medicare won’t have to pay more than $2,000 a year in out-of-pocket costs for prescription drugs, which will make a big difference for seniors with certain conditions like cancer and multiple sclerosis. This would kick in in 2025.
And, starting next year, if drug companies raise the prices of their drugs faster than inflation, they’ll have to pay a rebate to Medicare. That could affect a lot of drugs – according to an analysis by the Kaiser Family Foundation; in 2019-20, half of all prescriptions covered by Medicare increased in price faster than inflation. This provision could help discourage drug companies from constantly hiking prices.
Do experts think it will make a difference?
Actually, many health policy experts think these changes are significant.
“This is a huge breakthrough,” says Tricia Neuman, who directs the Program on Medicare Policy at KFF. “Congress has been talking about doing something about drug prices for decades. [This] may not be everything everyone wants, but it really is a big deal and it will provide significant help to literally millions of people who need it.”
“It’s a huge deal,” agrees Stacie Dusetzina, professor of health policy at Vanderbilt University. “It really does break a lot of new ground and fix a lot of problems.”
The Congressional Budget Office, which analyzed an earlier version of the bill, estimates these changes will save the government $288 billion through 2031.
Why does it take so long for many of these things to kick in?
For someone who’s on Medicare and spends $10,000 a year on cancer treatment, like Neuman’s friend, the timeline of these changes might be tough to take.
“Clearly, she’ll be wondering next year, ‘Why am I still paying a lot of money?'” Neuman says. “Some things just can’t happen fast enough just because it takes a while to put things in motion.” It will take a lot of work by the federal health agencies and industry groups to get ready for these provisions to take effect.
Neuman says she understands people are anxious for relief, but once provisions like the out-of-pocket cap in Medicare do take effect, “this really will be a big deal for people who rely on expensive medication and for others who have seen their drug prices increase each year.”
I heard the bill will lead to fewer new drugs. Is that true?
This is an argument made by drugmakers to try and scare people into opposing these changes. The pharmaceutical and health products industry has spent more on lobbying Congress in 2022 than any other industry, according to the nonprofit Open Secrets. It’s fighting hard to prevent these changes from becoming law because they would cut into their profits.
For instance, PhRMA, the Pharmaceutical Research and Manufacturers of America, is making its case in an ad campaign that the drug-pricing provisions in the bill could lead to fewer new medicines coming to market by “chilling research and development.” The trade association also pointed NPR to this industry-funded analysis from Avalere, which estimates the bill could reduce drug manufacturer revenue by $450 billion by 2032.
But an analysis by the Congressional Budget Office estimates the effect on drug development would be quite modest. About 15 out of 1,300 drugs would not come to market over the next 30 years – that’s about 1% of new drugs. Also, most big drug companies spend more on marketing than on research and development.
Some ads claim Medicare would be cut. Is this true?
These ads are misleading. For example, a project dubbed Commitment to Seniors launched a seven-figure ad campaign claiming that the Senate bill would “siphon nearly $300 billion out of Medicare.” In fact, that amount of money is what the government is expected to save because Medicare won’t have to pay as much for expensive drugs, it’s not money that’s being taken away from Medicare’s budget. So, importantly, seniors’ benefits would not be cut.
“When people see an ad on TV from a group called Commitment to Seniors, that sounds pretty innocuous,” says Michael Beckel of Issue One who tracks dark money. It turns out, Commitment to Seniors is a project of another group, American Commitment, that has given PhRMA more than a million dollars, including $325,000 in 2020.
Beckel says it’s not unusual to see the industry engage in such tactics. “The pharmaceutical industry is a major lobbying force and major dark money player.”
What about insulin? Would people with diabetes get help with those prices?
Insulin is often the poster-child drug when it comes to out-of-control prices and life-or-death stakes. U.S. insulin prices are four times higher after rebates, on average, compared with other countries, and about 1 in 4 diabetes patients has reported taking less insulin than prescribed because they can’t afford it. At this point, it’s unclear if any of the proposed reforms on the price of insulin – or at least patients’ out-of-pocket costs – will make it into the final bill.
A provision to cap copays at $35 a month for people with insurance who take insulin has bipartisan support, but may not be included in the final bill.
What else is in the bill on health?
The other big thing in the bill protects consumers from a potentially disastrous change that would happen without new legislation.
People who buy insurance on the Affordable Care Act marketplaces – like Healthcare.gov and the state marketplaces – will be able to keep generous premium subsidies for three more years. After these extra subsidies went into effect with the passage of the American Rescue Plan, the government estimated 4 out of 5 enrollees qualified for a plan with a premium of $10 or less per month.
Krutika Amin, who works with Neuman at KFF, says it’s important for lawmakers to nail down this extension now, since insurance companies are currently setting their rates for next year’s plans in advance of open enrollment in the fall.
“If Congress is able to extend the extra subsidies before the August recess, it will help provide certainty to both insurance companies and state and federal agencies who are running [the marketplaces] to be able to implement it in a way that’s seamless for consumers,” she says.
The extra discounts on plans have made a difference. Last year 14.5 million people – more than ever – signed up for insurance on Healthcare.gov, and an early analysis from HHS suggests the overall number of people who were uninsured in the U.S. hit a record low in the first months of this year.
NPR Pharmaceuticals Correspondent Sydney Lupkin contributed reporting.
[ad_2]
Source link