
[ad_1]
New suggestions spotlight potential advantages.
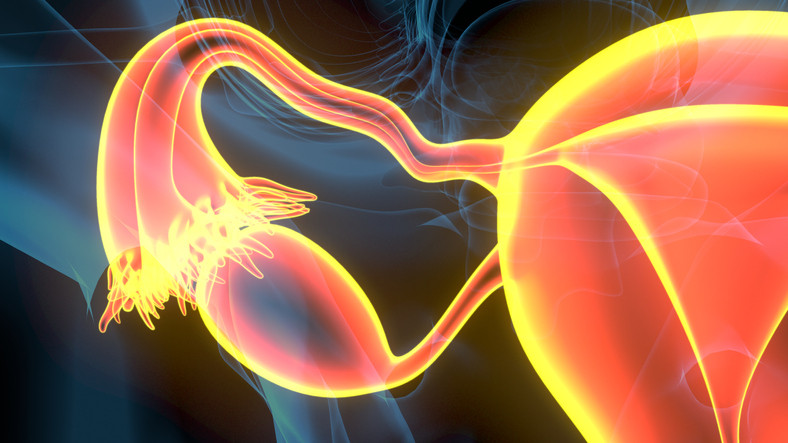
Should a lady think about having her fallopian tubes eliminated to decrease her danger for creating ovarian most cancers? Recent recommendations from the Ovarian Cancer Research Alliance (OCRA), endorsed by the Society for Gynecologic Oncology, encourage this technique, if girls are completed having kids and can be present process gynecologic surgical procedure anyway for different causes.
Why is that this new steerage being provided?
Ovarian most cancers claims about 13,000 lives each year, in line with the American Cancer Society. The new steerage builds on established recommendation for girls with high-risk genetic mutations or a powerful household historical past of ovarian most cancers.
This concept is not new for girls at common danger for ovarian most cancers, both: in 2019, the American College of Obstetricians and Gynecologists (ACOG) floated this technique in a committee opinion.
A Harvard professional agrees the strategy is sound, contemplating established proof that many instances of aggressive ovarian cancers come up from cells within the fallopian tubes.
“We’ve known for a long time that many hereditary cases of ovarian cancer likely originate in lesions in the fallopian tubes,” says Dr. Katharine Esselen, a gynecologic oncologist at Beth Israel Deaconess Medical Center. “Although we group all of these cancers together and call them ovarian cancer, a lot actually start in the fallopian tubes.”
Can ovarian most cancers be detected early via signs or screening?
No — which helps gas these suggestions.
Ovarian most cancers is notoriously tough to detect. Symptoms are typically obscure and may very well be associated to many different well being issues. Signs embrace bloating, pelvic ache or discomfort, adjustments in bowel or bladder habits, feeling full earlier when consuming, fatigue, uncommon discharge or bleeding, and ache throughout intercourse.
Disappointing outcomes from a big 2021 examine within the United Kingdom reported in The Lancet present that reducing the dangers of a late-stage analysis is not straightforward. The trial tracked greater than 200,000 girls for a mean of 16 years. It discovered that screening average-risk girls with ultrasound and a CA-125 blood check would not cut back deaths from the illness. By itself, the CA-125 blood check is not thought-about dependable for screening as a result of it isn’t correct or delicate sufficient to detect ovarian most cancers.
Only 10% to twenty% of sufferers are recognized at early levels of ovarian most cancers, earlier than a tumor spreads, Dr. Esselen notes. “There’s never been a combination of screenings that has reliably identified the majority of these cancers early, when they’re more treatable,” she says.
What does it imply to be at increased danger for ovarian most cancers?
Family historical past is the highest danger issue for the illness, which is recognized in practically 20,000 American girls yearly. A girl is taken into account at increased danger of ovarian most cancers if her mom, sister, grandmother, aunt, or daughter has had the illness.
Additionally, inherited mutations within the BRCA1 or BRCA2 gene elevate danger significantly, in line with the National Cancer Institute. (These mutations are more common among certain groups, together with folks of Ashkenazi Jewish heritage.) While about 1.2% of ladies general will develop ovarian most cancers of their lifetime, as much as 17% of these with a BRCA2 mutation and as much as 44% with a BRCA1 mutation will accomplish that by ages 70 to 80.
How a lot can surgical procedure decrease the percentages of ovarian most cancers?
It’s not clear that all girls — even these not scheduled for surgical procedure — ought to bear elimination of their fallopian tubes to scale back this danger as soon as they end having kids, Dr. Esselen says. This surgical procedure cannot completely eradicate the potential of ovarian most cancers — and surgical procedure carries its personal dangers. She recommends discussing choices together with your physician relying in your degree of danger for this illness:
For these at common danger for ovarian most cancers: Available information appear to help the thought of eradicating the fallopian tubes. Studies of ladies who underwent tubal ligation (“tying the tubes”) or elimination to keep away from future pregnancies point out their future dangers of ovarian most cancers dropped by 25% to 65% compared to their peers. And if a lady is already present process gynecologic surgical procedure, akin to a hysterectomy, the potential advantages possible outweigh the dangers.
Before menopause, eradicating the fallopian tubes whereas leaving the ovaries in place is preferable to eradicating each. That’s as a result of estrogen produced by the ovaries may help shield in opposition to well being issues akin to heart problems and osteoporosis. Leaving the ovaries additionally prevents immediately experiencing signs of menopause.
“The fallopian tubes don’t produce any hormones and aren’t really needed for anything other than transporting the egg,” she says. “So there’s little downside to removing them at the time of another gynecologic procedure if a woman is no longer interested in fertility.”
For these at excessive danger for ovarian most cancers: “In a world where we don’t have good screening tools for ovarian cancer, it makes sense to do something as dramatic as surgery to remove both ovaries and fallopian tubes when a woman is known to be at higher risk because of a strong family history or a BRCA gene mutations,” Dr. Esselen says.
Currently, preliminary proof suggests it could be protected to proactively take away the fallopian tubes whereas delaying elimination of the ovaries to nearer to the time of menopause to keep away from an early menopause. However, it is unclear how a lot this process lowers the percentages of creating ovarian most cancers.
“Generally, the findings so far have focused on the safety of the surgery itself and women’s quality of life,” Dr. Esselen says. “Long-term data in high-risk women takes a great number of years to accumulate. We need this data to know whether removing the fallopian tubes alone is equally effective in preventing ovarian cancer as removing the tubes and ovaries.”
Discussing your choices is vital
Ultimately, Dr. Esselen says that she advocates OCRA’s new suggestions. “For anyone who’s completed childbearing, if I’m doing surgery that wouldn’t necessarily include routinely removing their fallopian tubes, I’m offering it,” she says. “A woman and her doctor should always discuss this at the time she’s having gynecologic surgery.”
[adinserter block=”4″]
[ad_2]
Source link