
[ad_1]
Pancreatic most cancers is a kind of most cancers that develops within the pancreas, an organ situated behind the abdomen that performs an important position in digestion and the regulation of blood sugar. Pancreatic most cancers is sometimes called a “silent killer” as a result of it typically goes undetected till it has superior and unfold to different components of the physique. Symptoms of pancreatic most cancers embrace jaundice, belly ache, weight reduction, and blood clots.
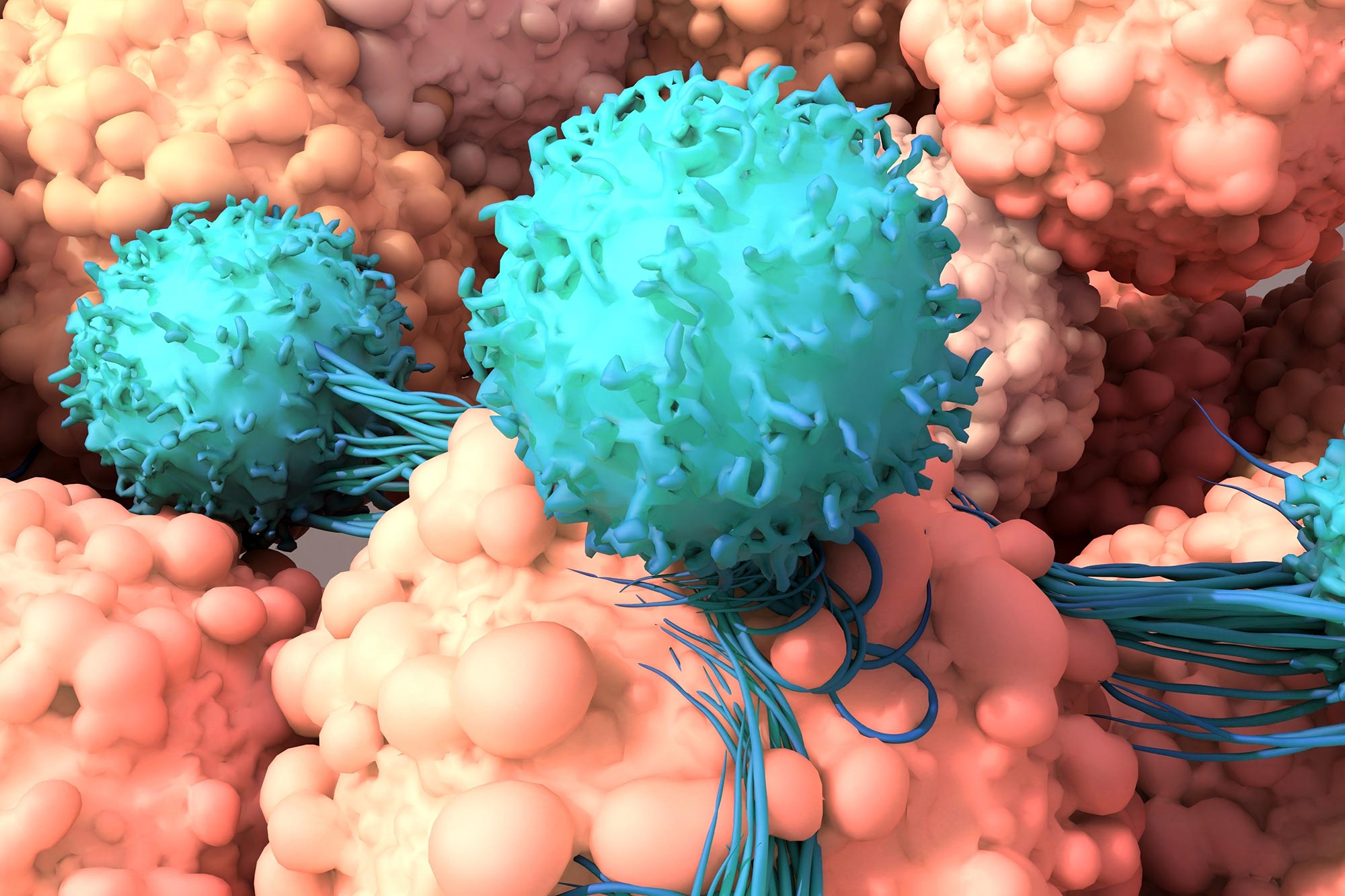
A brand new immunotherapy releases cancer-killing cytokines solely throughout the tumor.
Researchers on the University of California San Francisco (UCSF) have developed a brand new T cell-based immunotherapy that selectively targets most cancers cells, producing a strong anti-cancer cytokine particularly when it encounters tumors. This remedy successfully eradicated melanoma and pancreatic most cancers in mice, with minimal negative effects. This represents a promising new method for treating these and different difficult-to-treat cancers.
The cells ship IL-2, a naturally-occurring inflammatory molecule produced by the immune system that has highly effective anti-cancer results. It supercharges T cells, that are immune cells that may remove most cancers cells and battle an infection. IL-2 potent anti-cancer results have been long-known, nonetheless, systemic administration of IL-2 has been restricted as a result of extreme negative effects it could trigger.
In the research, which was just lately revealed within the journal Science, the researchers have been capable of maintain the cytokine contained throughout the most cancers by programming the tumor-infiltrating T cells to make their very own IL-2 once they acknowledged a most cancers cell.
“We’ve taken advantage of the ability of these cells to be local delivery agents and to crank out their T-cell amplifiers only when they recognize they’re in the right place,” mentioned Wendell Lim, Ph.D., the Byers Distinguished Professor in mobile and molecular biology, director of the UCSF Cell Design Institute and senior creator on the research. “I think this is a model for how we can use cell therapies to deliver many types of potent but toxic therapeutic agents in a much more targeted manner.”
Slipping previous the limitations
Cellular therapies have been extremely efficient towards many blood cancers, the place the cells are simply accessible as a result of they’re floating freely. Solid tumors, nonetheless, construct a number of defensive partitions that forestall therapeutic T cells from getting into. And even when the cells do get into the tumor, they typically tire out earlier than they’re capable of end off the cancerous cells.
Since the Eighties, oncologists have identified that prime doses of IL-2 allow T cells to beat these limitations, and the cytokine has been used as a most cancers remedy in difficult most cancers instances. But merely infusing sufferers systemically with IL-2 could cause excessive fever, leaky blood vessels, and organ failure.
Lim and lead creator Greg Allen, MD, Ph.D., adjunct assistant professor of drugs and a fellow on the Cell Design Institute, aimed to tame IL-2’s results by engineering cells that improve the cancer-killing immune response solely the place it’s wanted: within the tumor.
They selected to go after notoriously difficult-to-treat tumors, like these of the pancreas, ovary, and lung, that kind almost iron-clad limitations towards T cells.
To engineer cells T cells that would sense once they have been within the tumor, the researchers used an artificial Notch (or synNotch) receptor, a versatile sort of molecular sensor, which Lim’s lab developed a number of years earlier. These receptors span the cell membrane, with ends that protrude each inside and out of doors the cell. The exterior portion acknowledges and binds to tumor cells, triggering the within portion to set the manufacturing of IL-2 in movement.
The group examined the synNotch cells on quite a lot of lethal tumors, together with melanoma and pancreatic most cancers, and located that the cells labored precisely as deliberate.
“We were able to design these therapeutic cells to slip past the tumor’s defensive barriers. Once in the tumor, they could establish a foothold, and begin effectively killing cancerous cells,” mentioned Allen. “We got on top of these tumors and in some cases cured them.”
A Positive-Feedback Circuit
The method owes its success to engineering a circuit within the cell that amplifies the immune response in a managed approach. This induces the cell to provide IL-2 solely below the precise situations it’s programmed to acknowledge.
“This induction circuit is really a positive-feedback loop, an important element behind making these designer T cells that are able to operate so effectively,” Allen mentioned.
The circuit begins when the synNotch receptor tells the T cell to make IL-2. That IL-2 feeds again on the cell, inflicting it to divide, in flip creating extra cells that make much more IL-2. The total course of is confined throughout the tumor, defending the remainder of the physique from hurt.
Allen, who’s each a researcher and an oncologist, hopes to start testing the therapeutic method in medical trials with pancreatic most cancers sufferers in 2024.
“The most advanced immunotherapies are just not working in a lot of these difficult solid tumors,” he mentioned. “We think this type of design can overcome one of the major barriers and do it in a way that’s safe and free of side effects.”
Reference: “Synthetic cytokine circuits that drive T cells into immune-excluded tumors” by Greg M. Allen, Nicholas W. Frankel, Nishith R. Reddy, Hersh Ok. Bhargava, Maia A. Yoshida, Sierra R. Stark, Megan Purl, Jungmin Lee, Jacqueline L. Yee, Wei Yu, Aileen W. Li, Ok. Christopher Garcia, Hana El-Samad, Kole T. Roybal, Matthew H. Spitzer and Wendell A. Lim, 16 December 2022, Science.
DOI: 10.1126/science.aba1624
The research was funded by the National Institutes of Health.
[adinserter block=”4″]
[ad_2]
Source link